Abstract
Introduction Venous thromboembolism (TE) is a well-recognized complication of cancer, both in pediatric and adult populations. Adult oncology studies indicate a possible negative association between venous TE and survival. Despite pediatric patients with acute lymphoblastic leukemia (ALL) being at higher risk for TE, the association between TE and survival has been insufficiently examined. This systematic review investigates the following question: Within pediatric (0-18 years old) and adolescents and young adult (18-39 years old) (AYA) patients with ALL, what is the impact of the development of TE on the overall survival (OS) and event-free survival (EFS) compared to those without TE?
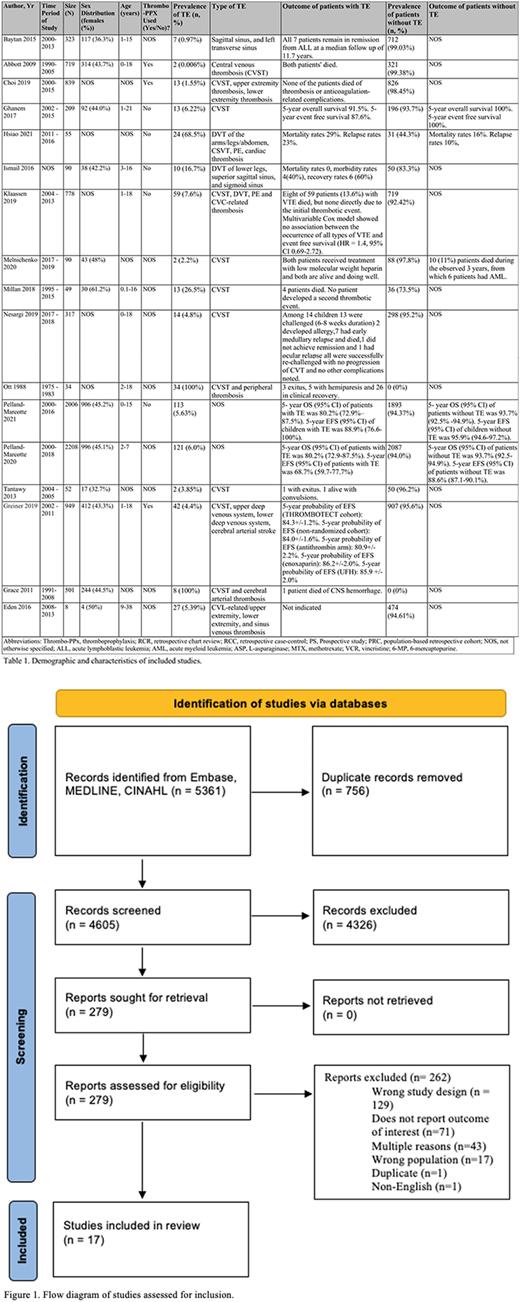
Methods A comprehensive search strategy was developed in Embase, MEDLINE, and CINAHL databases (accessed June 14, 2021). Original research papers in English reporting the OS and EFS of pediatric and AYA population with ALL and TE were included. To ensure reliability, two reviewers independently screened titles, abstracts, and full-text articles for inclusion. Conflicts were resolved by a third member and through further discussion with the team. This systematic review's protocol was approved by PROSPERO.
Results Our electronic search identified 5361 unique citations (Figure 1). Following the exclusion of duplicates, 4605 titles and abstracts were screened. Of these, 4326 studies did not meet the inclusion criteria and 279 full-text studies were screened further. Of these, 17 studies met the inclusion criteria and were included in this systematic review.
Demographic data of the included studies can be found in Table 1. From the seventeen included studies, 10 were retrospective chart review, one was a retrospective case-control study, four were prospective studies, and two were population based retrospective cohort studies. The majority of the included studies (n=15, 88%) had TE as a primary or secondary aim. All included studies had patient populations with ALL, and two of these studies had additional patients with acute myeloid leukemia.
From the seventeen included studies, a total of 9227 patients were included in this systematic review, of which 504 patients developed TE, corresponding to a prevalence of 5.46%. Overall, thirteen of the included studies provided mortality as a categorical variable; however, eleven of these thirteen studies only provided this data for those with TE. Of the eleven studies, which included 504 patients with TE, 33 patients died, corresponding to a mortality rate of 6.55%. Four of the included studies provided EFS and OS as the primary outcome, however, only three of these studies provided these outcomes for both patients with and without thromboembolism. Crude analysis of these three studies, which included 4423 patients, revealed an OS of 83.97% and EFS of 81.73% for those with TE, compared to OS of 95.8% and EFS of 94.83% for those without TE.
Conclusion While a meta-analysis of the included studies in this systematic review could not able to be performed given the heterogeneity of the studies, we did identify a lower survival rate in the TE population, compared to the population without TE, as evidenced by the relatively lower OS in the TE population, as well as the corresponding mortality rate of 6.55%. Many of the included studies had varying definitions for survival, and inconsistently reported the survival data for both populations with and without TE. Indeed, only four of the included studies provided EFS and OS as outcomes and the remaining thirteen studies provided categorical data, including survival rates, and mortality rates. We recommend that future studies should include consistent definitions of survival, and such data should be provided for both populations of patients with and without TE. Additionally, we intended to conduct a subgroup analysis on AYA population, as this often is an under-studied population. Unfortunately, only one of the seventeen included studies provided data on AYA population. We thus recommend future studies investigating outcomes of TE in ALL patients, specifically include AYA populations.
Discussion This review's strengths include its comprehensive search strategy created in consultation with a health sciences librarian, and a protocol that was established a priori. One limitation is our inclusion of solely English studies, thus limiting the data retrieved from non-English speaking countries.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.